As a general rule, the most successful man in life is the man who has the best information.
People with insulin-dependent diabetes (all of type-1 and about 27 percent of type-2 diabetics) lack the necessary amount of insulin in their bloodstreams. This can and often does lead to irreversible damage to their hearts, blood vessels, eyes, kidneys, skin, feet and hearing. In individuals taking insulin injections to reduce blood sugar levels severe hypoglycemia can cause organ failure and death.
Paul Lacey was a researcher at Washington University when, in 1972, he cured some diabetic rats by transplanting the islet cells from healthy rats into diabetic ones.
Over the next two decades researchers made hundreds and hundreds of attempts to apply the procedure to humans. Unfortunately no one was successful. By the early 1990's most scientists had come to the conclusion that islet-cell transplantation was a lost cause.
Dr. James Shapiro, Dr. Jonathan Lakey and colleagues from the University of Alberta in Edmonton developed the Edmonton protocol in the late 1990s.
The Edmonton Protocol is a method of implantation of pancreatic islets into the portal vein of the recipient's pancreas. These pancreatic islets are sourced/extracted from pancreases removed from recently deceased adults.
Each recipient receives islets from one to three donors. The islets are infused into the patient's portal vein, and are then kept from being destroyed by the recipient's immune system through the use of two immunosuppressant drugs as well as an antibody drug specifically used in transplant patients.
Dr. Shapiro and Dr. Lakey reported Edmonton protocol patient outcomes in the September 28, 2006, issue of the New England Journal of Medicine (NEJM): out of thirty-six patients transplanted, sixteen or 44 percent were insulin-independent after one year. Another 10 percent of patients were able to reduce the number of insulin injections they needed each day and the remaining 10 patients had totally rejected the transplant islet cells.
Since 2000 several hundred people have received islet transplants - but by five years after the procedure, fewer than 10% of all patients are free of daily insulin supplementation.
DR. JAMES SHAPIRO, MD, Ph.D. FRCS (Eng.) FRCSC, JOINS SERNOVA SCIENTIFIC ADVISORY BOARD
Sernova Corp. (TSX-V: SVA), is pleased to announce the appointment of Dr. James Shapiro, MD, Ph.D. FRCS (Eng.) FRCSC, to the Corporation's Scientific Advisory Board. In 2000, Dr. Shapiro led the team responsible for developing the Edmonton Protocol which was a major advancement in the treatment of insulin-dependent diabetes and now the current standard of care for Islet Transplantation.
Dr. Shapiro, a world-renowned transplantation scientist and clinician is Director of the Clinical Islet Transplantation Program at the University of Alberta where he oversees the largest clinical islet transplant program in the world.
"I am very impressed with the preclinical assessment of Sernova's Cell Pouch System™ and look forward to its clinical application." Said Dr. Shapiro.
Dr. Shapiro's research contributions have been principally focused on improving outcomes of clinical islet transplantation. Under his leadership, an extensive network of international collaborations has been developed to study islet function, and to monitor for tolerance and autoimmune reactivity in the islet recipients receiving immunosuppression. He is Principle Investigator on a number of US National Institutes for Health (NIH) and Juvenile Diabetes Research Foundation (JDRF)-funded clinical trials, including clinical testing of co-stimulation blockade in islet transplantation and he led an international multicentre trial of the Edmonton Protocol.
Dr. Shapiro has been the recipient of many awards, including a Hunterian Medal from the Royal College of Surgeons of England, the Gold Medal in Surgery from the Royal College of Physicians and Surgeons of Canada, and the Governor General's Gold Medal. He is a recipient of the Meritorious Service Medal from the Governor General of Canada.
He sits on the Editorial Board of the journal Transplantation and Diabetes Therapeutics and Technology, and is an active reviewer for several journals including Nature Medicine, Transplantation, and The British Journal of Surgery.
"The experience and clinical expertise of Dr. Shapiro will be invaluable to Sernova as it continues to plan its clinical trials program." Dr. Philip Toleikis, President & CEO
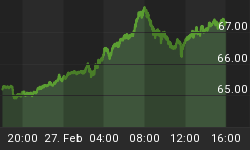
Sernova Corp. TSX.V - SVA
Common Shares: 78,953,824
Options: 3,396,375 average exercise price of $0.31
Warrants: 7,187,502 average exercise price of $0.20
Fully Diluted: 90,537,702
Insider Ownership: 6%
Sernova is developing two, novel, closely integrated, proprietary platform technologies. The first is the Cell Pouch System™ - a medical device providing a natural "organ-like" environment for therapeutic cells - such as insulin producing islets for diabetics. The second is Sertolin™ - a cell-based technology providing an immune-privileged environment for donor cells which reduces or eliminates the need for anti-rejection drugs.
The Standard of Care for patients with reduced or missing critical hormones or proteins, such as insulin, is often monitoring and injecting these proteins multiple times a day. This has lead to a patient track record of missing dosages and serious side effects resulting in US $150 billion a year hospital costs for diabetes alone.
Sernova's Cell Pouch System™ is a versatile, credit card-sized device made of FDA approved materials. Placed under the skin in a simple inexpensive procedure it develops into a tissue-engineered pancreas when islets are placed into the device. A key feature of the device is its ability to stimulate natural microvessel development, thought to be essential for long-term survival and function of therapeutic cells.
Cell therapy (a projected yearly US $8 billion market) is a new and increasing alternative for patients with severe disease.
At this time there is no approved device to house and protect therapeutic cells in the body. Instead, cells are often injected into vessels in an extremely expensive and risky procedure - most of the injected cells die from inflammation and clotting, an instant blood-mediated inflammatory reaction (IBMIR) - resulting in the need for reoperations. Currently cell therapy is limited to expensive procedures, poor cell survival and inappropriate delivery as well as lack of available donors.
Sernova's first application of its proprietary Cell Pouch System™ is islet transplantation for treatment of insulin-dependent diabetes - think of the Cell Pouch System™ as a potential natural insulin pump with the added benefit of fine-tuned glucose control. The Cell Pouch System™ is expected to prevent IBMIR (which is believed to rapidly destroy up to an estimated 90% of the transplanted islets) and in addition eliminate serious complications such as islet-induced blood clotting and liver thrombosis. The reduction in islet loss, once verified, could lead to improved safety and efficacy of islet transplantation and the potential of treating multiple patients from a single pancreas donation.
While the initial primary focus of the Company's development efforts will be assessment of the Cell Pouch System™ for insulin-dependent diabetes (which includes all Type-I diabetics and about 27% of Type-2 diabetics), the Company is planning to develop partnerships with academic and corporate collaborators to further develop the Cell Pouch System for other applications including:
-
Chronic metabolic, hematologic and neurological diseases - Parkinson's disease and Haemophilia are two candidates
-
Implantation of multiple cell types including natural cells, stem cells and genetically engineered cells
-
The Cell Pouch System™ may be used for autograft cellular transplants
-
Allograft cellular transplants with the use of immunosuppressive drugs or in conjunction with co-transplantation of islets and Sertoli cells
Sernova recently released interim results from a key porcine (pig) diabetes study evaluating the safety and efficacy of the Cell Pouch System™.
These interim results were presented at the American Society of Artificial Internal Organs 56th annual conference, Baltimore, Md., May 2009 and confirm that:
-
Sernova's Cell Pouch System™ establishes a biological environment capable of preserving the functionality of therapeutic cells
-
The Cell Pouch System™ allows for safe and efficacious cell-based therapy and may offer a revolutionary improvement over the current practice of injecting therapeutic cells into blood vessels
-
The Cell Pouch System™ can provide glucose control with only about 10% of the equivalent functioning islets that are used to achieve normal blood glucose levels in the current standard of care involving injection of cells into the veins suggesting that the device may be islet-sparing
Long-term efficacy results from the study were just presented at the XXIII International Transplantation Conference in Vancouver, B.C., August 2010. Results demonstrated a good safety profile and that the Cell Pouch System™ was able to eliminate the need for insulin injections in a number of animals for the duration of the study which was over 70 days. Furthermore, the study demonstrated clear evidence of significant micro vessel growth around the islets within the Cell Pouch System™, a key feature thought to be essential for long-term survival of the islet grafts.
Sernova's second technology, Sertolin™, is for patients who have had therapeutic cell therapy and who want to avoid toxic and expensive anti-rejection drugs (US $10-15,000/yr). Sertolin™, when combined with therapeutic cells protects them from attack by the immune system. Animal models have shown that the combination of these protector and therapeutic cells leads to long-term functional survival of the therapeutic cells without drug therapy.
Conclusion
There is no market cycle for bio-technology drug or device stocks. The need is always there and demand is growing at an alarming rate. More and more people are receiving medical coverage while at the same time big pharma's number of patents and pipeline of new drugs has been drastically reduced.
Dr. Shapiro joining Sernova's advisory board is a huge confidence boost for the company's technology. Sernova should be on every investor's radar screen.
Is it on yours?
Richard Mills owns shares in Sernova.
Sernova Corp. TSX.V - SVA is an advertiser on his website aheadoftheherd.com
If you're interested in learning more about the bio-tech sector and the junior resource market please come and visit us at www.aheadoftheherd.com. Membership is free, no credit card or personal information is asked for.