Worldwide, tens of thousands of researchers are working feverishly on a cure for cancer, testing countless new drugs and dozens of novel approaches. Most will end up in the dustbin. But among the most promising of that small group likely to make it to market is monoclonal antibody therapy.
That may sound like a daunting scientific concept to try to wrap one's head around, but in essence monoclonal antibodies are simple. Most of us are familiar with antibodies, the road warriors of the human body's immune system. They're those little Y-shaped proteins that are used to identify and neutralize foreign objects in the body (like bacteria and viruses) by binding themselves to the target - called an antigen - and killing it.
Although one antibody is generally very similar to another in structure, a small region at the tip of the protein is extremely variable - enough so that there are millions of distinct antibodies with slightly different tip structures, or antigen binding sites. This diversity allows the immune system both to recognize an equally wide variety of antigens and to come up with new responses to new types of infections.
Now, what if the body's ability to construct antigen-specific antibodies could be harnessed in the lab? What if scientists could produce substantial amounts of a single antibody (whichever one they wanted for a particular antigen) and that antibody alone, outside of the body? What if our own capacity for fighting infection could be turned against cancer cells? Wouldn't that be better than present chemotherapies, which willy-nilly blast diseased and healthy cells alike?
Of course it would. Making it happen is another matter.
Fortunately, many of the technical issues were resolved about 35 years ago, when Cesar Milstein, Georges Kohler, and Niels Jerne discovered how to fuse an antibody-producing cell with a cancer cell in the lab - an effort that won them the 1984 Nobel Prize in Physiology. The resulting mutant - dubbed a hybridoma - will produce large amounts of identical antibodies from a unique parent (that's the "monoclone" part) essentially forever.
The remaining challenge was how to put monoclonal antibodies to work against cancer.
What researchers came up with was elegant: To borrow from military parlance, they would create a "smart bomb," an antibody which - when combined with a cancer-killing drug - would detonate inside the diseased cell.
Though elementary in conception, the smart bomb was a long time in coming. First, an antibody had to be developed that would be accepted by the host and would navigate the bloodstream until it linked to a particular cancer cell. Then there would have to be a means for a potent cancer drug to be locked to it in such a way that the bond wouldn't disintegrate along the way; such a failure would create havoc among healthy cells. Finally, the antibody would have to be able to release its piggybacked drug once it reached its target.
The payoff is huge. Not only does this form of therapy allow for much more precise targeting, it permits the use of cytotoxins (cancer-killing agents) that are 100 to 1,000 times more potent than traditional chemotherapy drugs - a toxicity that would cause far too much collateral damage if they were introduced into the body in a non-specific way.
Fighting cancer with our own built-in defense mechanisms sounds both logical and at the same time improbable, since up to now we've had such little luck in combating the disease ourselves.
Yet that's the promise of monoclonal antibody therapy, and the good news is that today it is far down in the research pipeline. Much testing in human subjects has been done, with results among patients whose cancers were previously deemed intractable that are nothing short of spectacular.
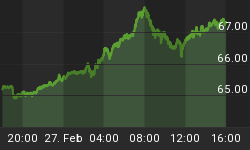
FDA clearance has been fast-tracked. The therapy has already been granted approval at the subcommittee level, with the full agency set to rule by the end of August. The first monoclonal antibodies with novel linkage systems binding to potent cytotoxins could hit the market this year, saving lives and making fortunes for both the company that developed them and those who invested in it.
Even the most diligent investor can't keep up with all the developments in cancer research, let alone build the knowledge necessary to understand both the promises and challenges they face. That's what makes a subscription to Casey Extraordinary Technology invaluable; the technology team does that work. And they've put together a curing cancer portfolio so that you can get in on the best prospects.