Today, personalized medicine seeks to move away from the one-size-fits-all, trial-and-error approach that has defined drug R&D and patient treatment basically since the time of Galen of Pergamon in the 2nd century AD. It increasingly focuses on matching the biological characteristics of each person with the best treatment options available and dosing for them, and in the future even perhaps the development of specific drugs for specific patients.
Truth be told, the idea of personalized medicine is nothing new. Back in the late 1800s, Canadian physician Sir William Osler (who was one of the founding professors at Johns Hopkins Hospital and has been called the "father of modern medicine") said, "Variability is the law of life, and as no two faces are the same, no two bodies are alike, and no two individuals react alike, and behave alike under the abnormal conditions which we know as disease."
Pathologists also often cite George Merck, who was talking about developing pharmaceutical agents directed toward individual patients rather than to groups of patients some sixty years ago, at the dawn of the era of personalized medicine.
Even though the idea has been around for some time, personalized medicine as a practice is quite new. Even just twenty years ago, virtually all drugs being developed attempted to target the entire population of a disease group rather than a subset or segment of it.
But all that is changing. Now, the development of drugs that are specifically linked to diagnostic tests that indicate a subgroup of patients is more likely to respond to treatment is often the goal for a variety of different diseases... particularly cancer.
Biomarkers are the key to this changing landscape in drug development and patient care. Biomarkers have the ability to help drug companies and physicians shrink costs, predict and minimize risk, avoid late-stage attrition, and make better, more informed decisions throughout the process. And they are poised to be the major driver of pharmaceutical research and drug development in the 21st century.
Originally, the term "biomarker" just referred to simple physiological indicators – such as body temperature, blood pressure, or heart rate – that signaled an imbalance in the body or evidence of disease.
Today, many different types of biomarkers have been identified by scientists. They still include things that are simple to measure and correlate, such as high blood pressure as an indicator for increased risk of stroke. But they also include more complex genetic changes or mutations that can, for instance, help identify a patient's risk for particular type of cancer. For example, mutations in the so-called BRCA genes are known to increase a woman's risk of developing breast or ovarian cancer.
Renowned oncology expert Dr. Jeffrey Ross defines a biomarker as "a series of gene sequences and mutations, messenger RNA expression profiles, tissue proteins, and blood based tests that can be used to detect the predisposition for disease, screen for its presence, confirm its diagnosis, assess its severity, predict its response to available therapies, and monitor its clinical course."
If that's not completely clear, Jeff Settleman from Genentech simply defines a biomarker as anything that can be measured as an indicator of a biological process. (A "biological process" can be something that is normally happening in the body, emerges during the development of a disease, or manifests in the response to a particular medicine in a patient undergoing treatment.)
A key takeaway from these definitions is that a biomarker is both objective and measurable.
In cancer research, biomarkers can be used to provide information about an individual's risk of developing the disease, his or her prognosis once the disease is diagnosed, and how he or she may respond to particular medications at various dosing levels – data that can be employed to better design a treatment regimen. Biomarkers can be prognostic, predictive, or in some cases both at the same time, offering the potential to inform treatment decisions and to bring more personalized medicine into clinical practice.
Ever-increasing development costs coupled with a rise in the failure rate for drugs in Phase II & III clinical trials has motivated big pharma and small biotech alike to incorporate biomarkers as an essential part of clinical development. At Genentech, for example, all new agents in its oncology pipeline include a corresponding biomarker program aimed at determining which patients are the best candidates for its clinical trials. Many pharma companies today would not even think of developing a new drug without simultaneously searching for biomarkers for safety, efficacy, and pharmacodynamics.
Biomarkers have the potential to accelerate product development and cut costs because they can help identify those drug candidates that are likely to fail sooner, and can predict drug efficacy faster than conventional clinical endpoints – giving life to the concept of "fail early, fail cheap." The FDA estimates that a mere 10% improvement in the ability to predict drug failures before clinical trials could save more than $100 million in development costs per drug.
One example from oncology of how biomarkers can help a drug company fail early and cheap comes from the use of circulating tumor cells (CTCs), a biomarker present in the blood of cancer patients. CTCs provide cancer-drug developers with an objective and direct measurement of the disease's response to a novel agent. According to Dr. Jeffrey Ross, chief pathologist at Albany Medical Center, this "can give a pharmaceutical company a very early signal of efficacy… If you're not knocking down the circulating tumor cells early in the trials, you may say, let's save our money for the next agent."
Some recent advancements in the study of biomarkers include:
- Researchers from the National Institutes of Health have linked the complement receptor-1 (CR1) gene with the risk of late-onset Alzheimer's disease.
- Researchers from Columbia University Medical Center have found potential biomarkers and drug targets for the more common, non-inherited form of Parkinson's disease.
- A group of scientists from the US, China, and Australia has found a marker that could inform doctors of the shift from normal skin cells to melanoma, potentially allowing for better screening and earlier diagnosis and treatment.
- German researchers have found an antibody in the blood of people with multiple sclerosis that could be a key to its diagnosis, as well as a clue to how it develops.
- A recent landmark study from a Canadian-UK consortium has used genetic biomarkers to split breast cancer up into 10 types, based on clusters of genetic markers, which could help predict which treatments would be most effective, and what the outcomes for patients are likely to be.
That's not to say that that the ushering in of an age of more personalized medicine through biomarkers is going to be easy. Just like with disease, there is no one-size-fits-all solution to biomarker discovery. Each potential candidate must be rigorously tested and validated; and the research needs to be interpreted carefully.
Still, the future of biomarkers looks bright. Herceptin (trastuzumab), Gleevec (imatinib mesylate), and Zelboraf (vemurafenib) are three cancer drugs on the market today that allow for a more personalized approach to treatment, thanks to the exploitation of genetic biomarkers. And in all likelihood, it won't be long before oncologists begin to use biomarkers to guide all aspects of care for patients with (or at risk of developing) cancer – with other medical fields following suit close behind.
From an investment perspective, there should be opportunities here. It might pay to dig into the publicly traded companies on the cutting edge of biomarker research and have a close-up look at what's going on in that space, rather than just focusing on existing drug pipelines and the market potential of those agents.
Biomarkers are just one of several amazing healthcare tech breakthroughs poised to give investors generous profits. Learn about another life-saving technology on the cusp of breaking in to the mainstream and get in on what may be the last chance to save 50% on the retail price of Casey Extraordinary Technology.
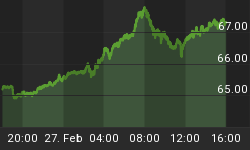
nd Stochastics