As the coronavirus pandemic continues to infect populations, though in some countries it is slowing, talk has shifted to re-opening economies, and to manufacturing a vaccine that drug companies hope will not only work, but can be distributed at large enough doses to provide immunity to a wide swath of the world's population.
In their daily media briefings, health officials dutifully trot out the number of cases for their particular area, how many hospitalizations have occurred, how many deaths, and how many have recovered from covid-19.
If there are signs of improvement, or “flattening the curve”, the next sentence invariably is about when tight social distancing measures can be loosened.
Researchers only recently started working on a vaccine, so realistically the earliest we could have one is the spring of 2021. Media reports over the weekend suggest that the US$50 billion vaccine industry, which is dominated by a few players, is “in an all-out sprint” to come up with one or more vaccines that will control the pandemic and put life back to normal.
At least 70 research teams, including some in Canada, are aiming to have a vaccine within a year. Progress has been slow, with only a handful of companies advancing from lab studies in animals to clinical trials in humans.
Despite unprecedented cooperation between pharmaceutical companies, the challenge is daunting because so little is known about covid-19. Unlike developing new vaccines for the flu, which is relatively well understood, or the 2009 H1N1 epidemic, whereby a vaccine was rushed out in six months,
“The difference [with H1N1] was that we had a vaccine and a production platform, we just had to make the doses,” the Globe and Mail quoted Clement Lewin, a 25-year veteran of the vaccine industry who now works for Sanofi S.A., one of the companies leading the race for a covid-19 vaccine.
“This is completely different because we’re developing the vaccine from scratch.”
The question for forward-thinking investors like us, and our subscribers, is what will the world look like after a vaccine is available? Will everything return to normal, as people are inoculated en masse? Will social distancing be remembered as just something we had to do, for a little while, until the virologists figured out how to beat covid-19? Or will the world have changed in profound ways we are just beginning to get a handle on?
At AOTH we are leaning towards the latter, based on what we know about vaccines, the history of pandemics, and some of the materials available for controlling the spread of viruses.
A pandemic timeline
Pandemics are capable not only of causing far-flung sickness, death and misery, but economic chaos due to the need for quarantines, the shutting of mines, factories, shops, really any workplace that can facilitate its spread, causing major disruptions to supply chains including delays, lost productivity, temporary closures or even bankruptcies.
What has been the deadliest disease in history? Going by the number of dead, mortality rate and speed of outbreak, the plague, cholera, smallpox and influenza are all contenders, but it was the 1918 Spanish Flu that tops the body count.
Between 1918 and 1920 the uber-deadly strain of influenza infected about 500 million people - an astounding third of the world’s population - and killed 20-50 million. The Spanish Flu had an extremely high mortality rate of 10 to 25%; in the first 25 weeks up to 25 million died. Mysteriously, this flu attacked not only the elderly, weak and very young, but healthy adults. It was not uncommon for an afflicted patient to be dead within a few hours of contracting the disease.
Three more flus make it into MPH Online’s grisly top 10 list of the worst pandemics. The 1889-90 Flu, otherwise known as the Asiatic or Russian Flu, was first observed in Central Asia, northwestern Canada and Greenland. It went global through urbanization, and is considered the first epidemic. The Asian Flu originated in China, in 1958. Its two-year spread resulted in about 2 million dead, including 69,800 in the United States. The Hong Kong Flu of 1968 was a fast-spreading H3N2 strain of the influenza A virus. It only took 17 days before outbreaks were reported in Singapore and Vietnam, and within three months cases were showing up in the Philippines, India, Australia, Europe and the US. Though it only had a 0.5% mortality rate, the Hong Kong Flu still killed over a million people including 500,000 residents of Hong Kong, about 15% of its population.
More recently we have the Avian Flu and Severe Acute Respiratory Syndrome (SARS). As the name suggests, the 1997 Avian Flu was spread through contact with infected poultry. From its first major outbreak in Hong Kong to the last in 2003, “bird flu” killed 257 - over 60% of those who contracted the virus.
SARS was a quick-moving virus that started in Guangdong province, China. In 2003, SARS spread to over 30 countries within a few months, infecting ~8,000 and killing 774. This compares to the coronavirus death toll of 177,148, as of this writing, out of over 2.5 million cases worldwide. About 645,000 patients had the respiratory illness but have recovered from it.
Then there’s cholera, particularly the Third and Sixth Cholera outbreaks, which killed a respective 1 million and +800,000. Transmitted by contaminated water, both cholera pandemics originated in India and (between them) spread to Asia, the Middle East, North Africa, Eastern Europe, Russia and America.
Going beyond flus, plagues and cholera, MPH puts HIV/ AIDS at the top of its list with a death toll of 36 million since 1981. While there are still between 31 and 35 million infected with HIV, new pharmaceutical treatments have prolonged lives.
The most resilient of pandemics is smallpox. Throughout its 12,000-year existence, smallpox has killed a mind-blowing 300-500 million people.
Ebola is often lumped in with historical pandemics, having ended over 11,000 lives, but because it is confined to West Africa, Ebola is considered an epidemic not a pandemic. It is still obviously a very serious disease.
The coronavirus is clearly far more deadly than SARS and the Avian Flu, but still quite a ways from the Sixth Cholera outbreak which resulted in 800,000 dead, or other influenza outbreaks whose body counts go into the millions.


Vaccines: No silver bullet
The most important number to know when it comes to ending a pandemic is the R0, pronounced “R-naught”. It refers to the average number of people one sick person goes on to infect, in a group that has no immunity. Experts use the R-naught to determine if an outbreak is taking off, leveling or diminishing. According to the World Health Organization, the R-naught of covid-19 is between 2 and 2.5, making it more contagious than the seasonal flu but less contagious than measels.
The current goal is to bring the R0 below 1, which would put the coronavirus in decline until it eventually dies out. Or will it? At this point covid-19 has infected so many people worldwide, it can no longer be compared to MERS or SARS, which both killed under 1,000. Instead, covid-19 is shaping up to be as bad or worse than the flu, which as mentioned, has had various iterations, some infecting populations in the millions. The two viruses may also share another characteristic: seasonality. It’s too early to say whether the virus will come and go with the seasons, however we do know it has the capability of re-infecting countries that had it under control. For example in March, Hong Kong saw a spike in cases due to travelers bringing the virus back into the country. The same thing happened in Singapore and Taiwan.
Along with lowering the R0 number, a pandemic is said to be brought under control when the population reaches “herd immunity”. This is the point when so many people have had the virus that they are immune, or when enough of the population has been vaccinated to prevent its spread.
According to Harvard epidemiologist Marc Lipsitch, the R0 of coronavirus is similar to the 1918 flu (!), meaning the end of the pandemic will require nearly 50% of the population either to become immune from a vaccine, or from natural infection, aka herd immunity.
That brings us to the topic of vaccinations. If the end game is to find a vaccine for covid-19, we need to ask an obvious question: How likely is it that a vaccine(s) would work to immunize half of the world’s population?
The influenza vaccine teaches the body to produce antibodies that fight the virus’ protein, called hemagglutinin (HA). However because the HA is highly mutable, a new formula must be manufactured each year.
Unfortunately, the success rate of the seasonal flu vaccine is not promising. Its effectiveness swings wildly from under 10% to at most 60%.
Despite comprehensive flu shot programs, the World Health Organization estimates the flu kills between 290,000 and 650,000 people a year. In the US, 12,000 to 61,000 deaths annually since 2010 were attributed to the flu.
In mid-February, the CDC reported via NBC News, there have been at least 26 million flu illnesses, resulting in 250,000 hospitalizations and 14,000 deaths, including 92 children.
The counter-argument might be that flu cases would be higher if there was no vaccine available. That only holds true if the success rate is consistent. The data shows otherwise. One problem is that flu viruses change. As they move from one host to another, over time the mutated virus is no longer recognizable to the flu vaccine. When this happens during the flu season, the vaccine people got in November fails to work against the new strain.
For example, the 2018-19 flu vaccine was no match for a particularly vicious end-of-season flu, which dragged its effectiveness down to 29%.
And while the success rate of the current flu shot (designed for two strains, A/H1N1 and B/Victoria) is more effective, 45%, against A/H1N1 it is only 37%, and for adults 18 to 49 battling type A, it offers virtually no protection. Against type B the vaccination is 50% effective.
According to Michael Osterholm, an epidemiologist at the University of Minnesota quoted by Science magazine, 10 % to 60% is surely better than nothing, “But it's a terribly inadequate vaccine for a serious public health threat.”
In the early days of the pandemic, a lot of people pointed to the large number of people killed from the flu as evidence the new coronavirus was no big deal. We now know it to be 10 times more deadly, at 0.1% mortality for the flu vs 1% for covid-19.
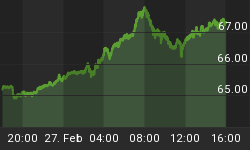
The WHO numbers above show the seasonal flu killing 61,000 Americans a year at the high end; so far this “covid-19 season”, if we may call it that, 42,514 have died. But the United States is nowhere near flattening the curve, compared to its country peers on the graph below, suggesting the number of covid-19 deaths this year could easily reach parity with the number who die from the flu in a particularly bad season.

The new normal
How would a covid-19 vaccine fare against a virus that has shown to be far more deadly than the seasonal flu? I don’t like its chances. As with flu vaccines, if scientists come up with a working vaccine, but the coronavirus mutates, it would render said vaccine useless.
Moreover, there has never been a successful vaccine for a coronavirus. To find out why, read a story from Australia’s ABC News, quoting scientist Ian Frazer from the University of Queensland. Dr. Frazer helped develop the vaccine for the human papilloma virus which causes cervical cancer. On coronavirus immunity he states,
“It's a separate immune system, if you like, which isn't easily accessible by vaccine technology,” Professor Frazer told the Health Report...
"One of the problems with corona vaccines in the past has been that when the immune response does cross over to where the virus-infected cells are it actually increases the pathology rather than reducing it," Professor Frazer said.
Increases the pathology? That can’t be good. His pessimism is seconded by another scientist, David Nabarro, professor of global health at Imperial College London, and an envoy for the World Health Organization. As one of the world’s leading experts on covid-19, Dr. Nabarro is far from sanguine that a vaccine can be successfully developed, telling The Observer, via The Guardian, that humanity will have to live with the threat of coronavirus “for the foreseeable future.”
“You don’t necessarily develop a vaccine that is safe and effective against every virus. Some viruses are very, very difficult when it comes to vaccine development - so for the foreseeable future, we are going to have to find ways to go about our lives with this virus as a constant threat.
“That means isolating those who show signs of the disease and also their contacts. Older people will have to be protected. In addition hospital capacity for dealing with cases will have to be ensured. That is going to be the new normal for us all.”
Let us pause for a moment and let that sink in. Those who think we can just kill this thing and go back to hanging out in restaurants and bars, hopping on airplanes and comfortably swapping the same air as 300 other potentially covid-carrying passengers for up to 18 hours, crowding into sports stadiums cheek to jowel, are sadly mistaken. Even if a vaccine is developed, there is every possibility that preparing for it will become an annual event.
Temperature is one factor that determines whether or not a virus is seasonal. While it’s true that flu viruses tend to do better in colder, drier air found during winter months, tropical areas also have the flu even though they don’t have winter.
FiveThirtyEight, a statistical news site owned by ABC News, also reports that one of the biggest factors in whether a virus becomes seasonally recurrent, is whether it is pandemic (found everywhere) and endemic, meaning it is constantly circulating in human populations. The flu virus is both, therefore seasonal, and from FiveThirtyEight’s reporting, the same is likely to happen with the new coronavirus:
[Flu] doesn’t disappear every summer. It’s just biding its time, hanging out in human bodies (either at low levels of infection or in the opposite hemisphere), ready to spread again once conditions improve. SARS never became pandemic and endemic — largely because of a lot of human effort, and partly because of a convenient tendency to not be very transmissible until victims showed symptoms of infection.
But the new COVID-19 virus doesn’t seem to offer us that handicap. There seem to be asymptomatic cases, and mild ones that people don’t recognize as dangerous. And there’s evidence suggesting people can spread the virus before they’re even showing symptoms themselves. That makes it more challenging for public health experts to stop, Yang said. When I asked her how likely it was that COVID-19 could become seasonal, she laughed ruefully. “Nobody knows,” she said. “The WHO still says there’s hope we can get this under control.”
Right. The same WHO that China found a willing accomplice in repressing critical data on covid-19 that had it been released earlier, may have prevented an epidemic in China and a global pandemic from happening.
It’s worth remembering that all of this mess we’re currently in - stock markets crashing, oil futures going negative (!), a global depression gathering like an Oklahoma dust storm, millions of people thrown out of work, supply chains broken, front-line health workers dying for lack of PPE - was anticipated.
Coronavirus was not an “unforeseen problem” that “came out of nowhere,” as Donald Trump has stated. Repeated warnings about a flu-like pandemic being the highest-priority public health disaster to hit the United States, were dismissed or sat on by top US officials going back as far back as 2009.
The Director of National Intelligence regularly briefs Congress on the most serious threats facing the country. A recent article in Project Syndicate, entitled ‘The Spies Who Predicted COVID-19’, notes the DNI’s annual briefing kept warning about the risk of a pandemic. The first warning was sounded in 2009, immediately after Barack Obama took office, when then-DNI Dennis Blair testified that, “The most pressing transnational health challenge for the United States is still the potential for emergence of a severe pandemic, with the primary candidate being a highly lethal influenza virus.”...
Consider the 2008 report, “Global Trends 2025,” which was all but oracular. “The emergence of a novel, highly transmissible, and virulent human respiratory illness for which there are no adequate countermeasures could initiate a global pandemic,” the authors warned. The threat, they added, would likely emerge “in an area marked by high population density and close association between humans and animals, such as many areas of China and Southeast Asia.” Even with limits placed on international travel, “travelers with mild symptoms or who were asymptomatic could carry the disease to other continents.”
The Trump administration has been roundly criticized for being late to recognize how serious a threat the pandemic presented to the American public and economy, even as it was escalating in Asia.
An investigative report by ABC News reveals that intelligence bulletins concerning the virus began circulating around Thanksgiving (Nov. 28), the contents of which suggested that Beijing knew the coronavirus was out of control and was covering up its severity.
That same month, a report by the National Center for Medical Intelligence (NCMI) warned of a “cataclysmic event” now known as the covid-19 pandemic. Briefings of this report were sent to the Defense Intelligence Agency, the Pentagon’s Joint Staff and the White House.
It has also been pointed out that earlier resources, and one training exercise, put in place to deal with a pandemic of similar scope to covid-19, were either eliminated or ignored by the Trump administration.
A rumor that John Bolton, Trump’s former national security advisor and the National Security Council President in 2018, scrapped the pandemic preparedness office set up under Obama, was proven true by Snopes.
The team included Luciana Borio, the NSC’s director of medical and biodefense preparedness, who in May 2018 warned that a flu pandemic was the nation’s no. 1 health security threat. Borio left the Trump administration in 2019.
The White House also nixed a US public health position in Beijing tasked with helping detect disease outbreaks in China. The American epidemiologist, who was embedded in a Chinese health agency, left her post in July, 2019, depriving the US government of critical on-the-ground intelligence as the pandemic gathered speed in the first part of 2020.
Then there was the mock drill conducted by federal agencies in Chicago, in August 2019. The drill centered around how the nation would handle a global flu pandemic with no known cure. Prophetically, the outbreak begins in China and invades Chicago. NBC News reported the exercise, called ‘Crimson Contagion’, pointed to a number of national shortcomings, including an insufficient amount of medical supplies.
In a previous article we talked about how the White House botched the procedures for coronavirus testing, a key part of any pandemic response.
Most glaringly, President Trump denied he had ever seen two key memos about the coronavirus, written and circulated in January by Peter Navarro, his top trade advisor, and known China hawk.
The memos warned the covid-19 virus had the potential to kill hundreds of thousands of Americans, and cost the US economy trillions, unless tough actions were taken immediately. For more read Covid-19 - Who, what, when, where and why?
Preventing covid-19
If the coronavirus becomes seasonal like the flu, it stands to reason that taking proactive measures to avoid getting it - beyond getting vaccinated – is something we should all be looking at.
Everyone is now familiar with social distancing protocols, including staying at home, keeping 2 meters away from other people, and avoiding gathering in groups. Frequently washing hands for a minimum 20 seconds and not touching your face are also highly recommended.
But there are other things we can do to avoid getting sick - three areas to consider are the materials used to resist viruses, our lifestyle and our diet.
Medical and non-medical masks are among the most sought-after pieces of personal protective equipment (PPE) used to prevent the spread of covid-19. Hospital and care home workers on the front lines require N95 respirators - often in conjunction with face shields, gowns and rubber gloves - which reduce the wearer’s exposure to particles including aerosols and large droplets. The ‘95” means at least 95% of 0.3+ micron particles are filtered out. They are made of non-woven polypropylene fiber, and often have a valve to facilitate breathing. According to the Centers for Disease Control, tight-fitting N95 masks should be discarded after each patient encounter, and when they become damaged, contaminated, or no longer form an effective seal to the face.
By contrast surgical/ non-medical masks are loose-fitting face coverings that create a barrier between the mouth and nose and potential contaminants. If worn properly they protect the wearer from large droplets, splashes or sprays of bodily and other hazardous fluids. However they do not provide a reliable level of protection from inhaling smaller airborne particles and are not considered respiratory protection. The green surgical masks are a common sight these days among shoppers in confined spaces and for people who have a low risk tolerance for contracting the virus.
Disposable facemasks, both non-medical and N95, however can’t block all pathogens, meaning discarded masks can become vectors for disease.
This, along with chronic shortages of PPE including facemaks, has prompted research into decontamination methods for re-using N-95 respirators. In a recent National Institutes of Health study, scientists found that decontaminating N95 masks using vaporized hydrogen peroxide, 70-degree Celsius dry heat, UV light and 70% ethanol spray, effectively sanitized masks for limited re-use.
Meanwhile two Israeli companies are rushing to develop new antiviral masks that could be a powerful tool against flus and coronaviruses.
The technology invented by two Israeli chemistry professors, and being developed by Sonovia, infuses antiviral, antimicrobial zinc and copper oxide nanoparticles into textiles for facemasks and other protective products. According to Israel21C, tests have shown the treated textiles work against six types of bacteria including E.coli and Staph, and are effective for up to 100 washes at 75 degrees C. The masks appear to work against some strains of influenza but have not yet been proven for covid-19.
Picking up on the use of copper, it’s interesting to note that, while the coronavirus can survive for days on glass or stainless steel, it dies within hours after landing on the red metal.
That shouldn’t be a surprise for anyone with an understanding of copper’s antimicrobial effects. For thousands of years ancient peoples have known of copper’s disinfectant powers. An article in Smithsonian magazine states the first recorded use of copper as a pathogen-killing agent dates as far back as 3,200 BC, in ancient Egypt.
The Chinese used copper coins to treat heart and stomach pain around 1,600 BC and the Phoenicians inserted shavings from their bronze swords into battle wounds to prevent infection. For hundreds of years, mothers have known children who drink from copper vessels do not get diarrhea as frequently.
Remarkably, copper’s ability to stop diseases in their tracks does not appear to dissipate with time. Copper railings at New York City’s Grand Central Station were found to work just as well as when they were installed 100 years ago, Smithsonian said. The EPA has registered some 400 copper surfaces as antimicrobial.
This naturally leads into a discussion about whether copper could be used more in hospitals to reduce the spread of infections by touching common surfaces. A landmark study looked at copper alloys on various surfaces including bedside rails, tray tables and intravenous poles across three US hospitals. The 43-month investigation found a 58% reduction in infections compared to routine anti-infection protocols.
A further two-year study compared the surface of an intensive-care bed made from copper, to beds containing plastic. It found bed rails on plastic surfaces exceeded risk standards in 90% of samples, versus only 9% for the copper bed.
The Smithsonian notes health care systems in North Carolina and Virginia in 2017 made copper-impregnated surfaces the standard across 13 hospitals. One Virginia Beach hospital has even moved to copper-infused bedding using technology pioneered in Israel. Thanks to the red metal’s anti-microbial, anti-fungal and anti-odor properties, products/clothing containing copper are becoming more popular, including socks, shoe insoles, shirts and even dog beds.
The Conversation notes copper alloy touch surfaces are being deployed in airports, train stations, buses, restaurant kitchens, gyms, and even at one of the largest theme parks in Latin America, Fantasilandia in Chile.
Silver is also a strong contender for adapting to the new normal forced by the new coronavirus.
According to The Silver Institute,
Even before people fully understood how silver worked as an antibiotic, the metal was used to prevent the growth of dangerous germs. On long ocean voyages, for example, silver coins were dropped into water and wine casks to keep the liquids fresh. For decades, physicians placed several drops of silver nitrate into newborns’ eyes to prevent infection.
Related: Can Disney Bounce Back From Massive Coronavirus Loss?
During World War I, battlefields wounds were wrapped in silver foil and silver sutures were used to close deep wounds.
More recently, silver coatings are being placed on medical devices such as breathing tubes and catheters to help fight infections. It’s also being applied to artificial bones and scaffolding used to keep bones in place while they mend. Silver is found in bandages and ointments because it keeps bacteria at bay, allowing the body to heal faster.
Silver has also been shown to be effective against bacteria that are becoming resistant because of the overuse of chemical antibiotics. For example, a life-threatening Staph germ called MRSA (Methicillin-resistant Staphylococcus aureus), often referred to as a “superbug” and found in healthcare facilities, is resistant to almost all chemical antibiotics. To fight back, many facilities are employing silver-imbedded equipment including surgical tools, needles, stethoscopes, furniture, door handles, furniture, linens and even paper files.
The natural mineral silver can also be ingested to prevent viral infections. A daily dose of silver nanoparticles coats the surface of a virus in a way that prevents it from binding to healthy cells. Experiments in the 1980s found silver kills over 650 bacteria, fungi, parasites, molds and fungi that have the potential to sprout diseases - without side effects.
Conclusion
The virus that causes the common flu kills up to 650,000 people worldwide every year. Yet we take zero measures to prevent its spread, except for getting vaccinated against a virus that, at best, gives us 60% immunity and at worst under 10% protection. There is a strong likelihood that between vaccination and onset of flu symptoms, the virus will have mutated to the point where the vaccine is no longer effective.
We accept these 650,000 deaths from the flu, yet most countries have prevented all non-essential businesses from operating, confined people to their homes, and strongly discouraged them from traveling, all to slow the spread of the coronavirus which, at last count, has killed less patients than the flu – 177,148 vs an annual 290,000 to 650,000 flu deaths.
Yes, covid-19 is 10 times as infectious as the flu, but when a vaccine is found for it, will people keep follow social distancing measures? Likely not. There is no indication, especially in the US where social distancing is seen as an attack on civil liberties, that their behaviour will be any different from the seasonal flu, ie., except for a small minority of Asians, masks will not be worn in public, people will go back to coughing and sneezing on subways and elevators without covering their mouths, attending concerts, sports events, basically it will be business as usual despite at least 175,000 more deaths from coronavirus, and likely many more, considering the virus isn’t anywhere near contained.
The degree of covid-19 spread, now surpassing 2.5 million cases worldwide, combined with the fact that people can have mild symptoms or even be asymptomatic and still be “shedding virus”, makes it almost certain that coronavirus will become seasonal like the flu.
We can’t rely on a vaccine to protect ourselves. Remember, no vaccine has yet been successful against a coronavirus; the complexity of these viruses makes it difficult to trigger an immune response.
If we can’t rely on a shot for immunity, what else can we do? We can maintain social distancing, keep washing our hands (it’s a good practice to stop harmful bacteria even when viruses aren’t floating around), and always wear masks in high-risk areas like hospitals, health clinics, and nursing homes. Even flying/ rolling petri-dishes like airplane cabins and subway cars would be smart places to don a mask.
We can lobby governments and major medical suppliers like 3M to consider making facemasks that employ antimicrobial copper and silver - not only are copper-infused masks like those being trialed by an Israeli company more effective against bacteria and viruses, they can be washed and re-used up to 100 times. That’s better for the environment and reduces the supply of medical masks that have to be stockpiled.
Silver, already used in dozens of industrial applications, almost as many as oil, is another metal that could be tapped for helping slow the spread of existing and future, likely more deadly viruses. Applications include coating medical devices with silver to help fight infections, and ingesting tiny amounts of silver as an anti-viral supplement.
A lot of people take daily doses of Vitamin C to guard against colds and flus, and zinc to improve immunity and blood sugar levels. Vitamin D helps maintain a healthy immune system and helps protect against respiratory conditions.
The regular, seasonal onset of covid-19 is even more reason to continue taking these immunity-boosting supplements.
Diet is another largely neglected area when it comes to being proactive against potentially deadly flus and coronaviruses. Every doctor will tell you that eating a balanced diet with plenty of protein, less then 100 grams of carbs per day, fruits and vegetables, not smoking, and getting regular exercise (as simple as going for an hours walk every day), is a better prescription for good health than anything he can do for you.
Yet for many North Americans, that advice goes unheeded. A 2016 study found over half of Americans’ calories come from “ultra-processed” foods containing high amounts of sodium, trans fats and artificial sweeteners. They include white bread, potato chips, packaged snack cakes, frozen pizza, candy and soft drinks. Canadians and their regular outings to get fed through a hole in a brick wall aren’t doing any better.
Another landmark study compared the nutritional content of 43 fruits and vegetables in 1950 versus 1999. The results showed significant drops in the amount of protein, calcium, phosphorus, iron, riboflavin (vitamin B2) and vitamin C over a half-century. The “Green Revolution” may have succeeded in dramatically increasing crop yields, but at the cost of food quality. According to the World Watch Institute, you would have to eat 8 oranges today to derive the same amount of Vitamin C as our grandparents would have gotten from one.
Putting it all together, the conclusion is we all must take a much greater responsibility for our own healthcare than we currently are. Just as we can’t rely on the government for catching us when we fall from an economic disaster like covid-19 - every breadwinner should have at minimum three months of savings in the bank for a rainy day, and preferably, a stash of precious metals to serve as emergency currency in the event of a total financial system collapse - we need to become better prepared for pandemics.
At the very minimum I hope the current pandemic teaches people to: 1. Take personal responsibility towards maintaining your immune system by taking regular vitamin and micronutrient supplementation (always consult your doctor before starting any supplementation program) 2. Begin a healthier diet 3. Exercise regularly. These are the 3 key pieces of a virus-fighting strategy that should allow a greater degree of personal control in this new virus-controlled world.
Richard (Rick) Mills
More Top Reads From Safehaven.com: